Glomerulonephritis
How is glomerulonephritis diagnosed?
After checking your symptoms and medical history, your doctor will require some diagnostic tests, including:
- Urine test. This may show red blood cells and red cell casts in your urine, which is an indicator of possible damage to the glomeruli. The results may also show white blood cells that indicate infection or inflammation and increased protein that can reveal nephron damage. Increased blood levels of creatinine or urea are also red flags.
- Blood test. This provides information about kidney damage and impairment of the glomeruli. It is done by measuring levels of waste products, such as blood urea nitrogen and creatinine.
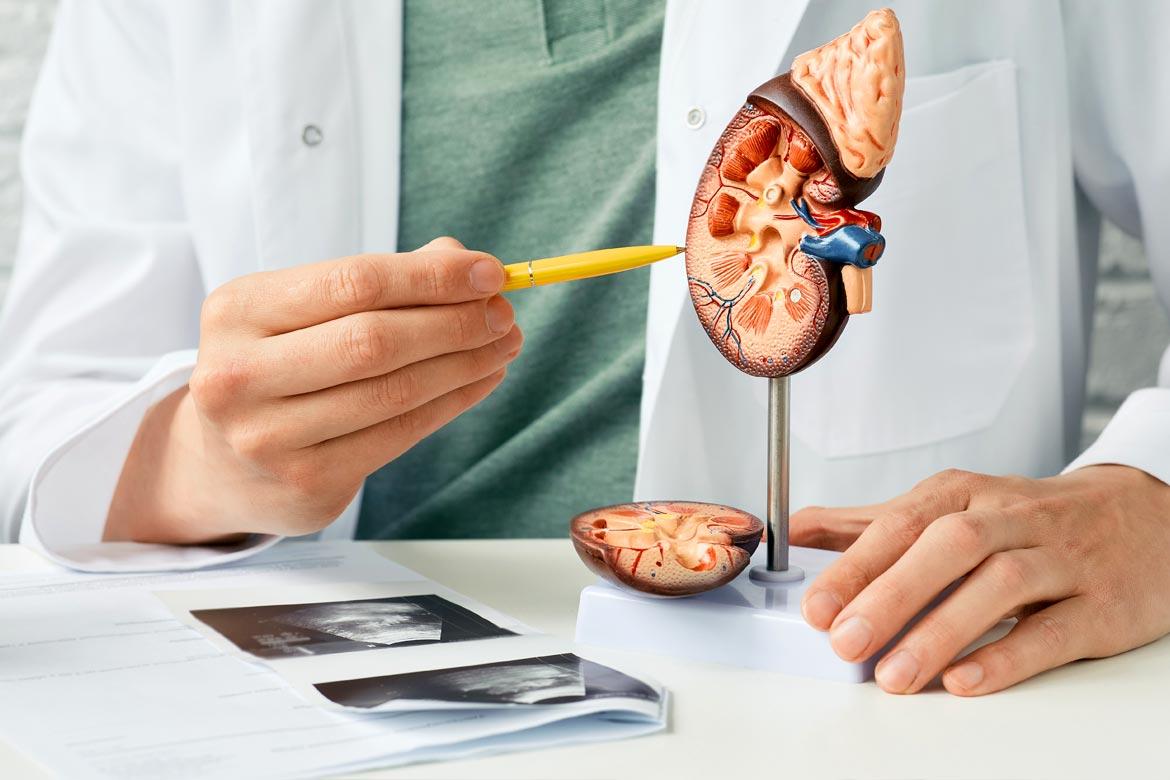
- Imaging tests. Your doctor may recommend diagnostic studies that allow visualisation of your kidneys. Imaging tests such as a kidney X-ray, an ultrasound exam, or a computed tomography (CT scan) are done if your doctor detects evidence of damage.
- Kidney biopsy. In a kidney biopsy, a special needle is used to extract small pieces of kidney tissue for microscopic examination. This is helpful in investigating the cause of the inflammation. This procedure is almost always necessary to confirm a diagnosis of glomerulonephritis.
How is glomerulonephritis treated?
Treatment options vary depending on the causes and severity of your symptoms. These include:
- Medications and therapeutics. Your doctor may prescribe blood pressure medications, such as angiotensin-converting enzyme (ACE) inhibitors. Angiotensin receptor blockers or ARBs, including losartan, irbesartan and valsartan, may also be prescribed. If your immune system is attacking your kidneys, corticosteroids and other medications to suppress the immune system may also be prescribed to reduce the immune response.
In addition, your doctor may also recommend plasmapheresis, a procedure to reduce immune-triggered inflammation. This method removes the fluid part of your blood, which is the plasma, and replaces it with intravenous fluids or donated plasma that contains no antibodies. - Dietary changes. Follow dietary changes advised by your doctor. This may include control of salt and water intake (to reduce fluid retention) and cutting back protein and potassium intake (to minimise waste accumulation in the body).
- Surgery. If your condition becomes advanced and you develop kidney failure, dialysis or other forms of treatments to replace kidney function might be needed. Dialysis can help remove excess fluid and control high blood pressure for glomerulonephritis. When a kidney transplant is not possible due to poor general health or other reasons, haemodialysis, in which a machine filters your blood or peritoneal dialysis (also called water dialysis), may be the only options for active management.
Conservative care or palliative care may be considered in select situations based on the patient's condition and preferences.
This page has been reviewed by our medical content reviewers.
Need help?
For enquiries, please call
+65 6250 0000 (Orchard) or +65 6898 6898 (Novena)
For appointment bookings, please WhatsApp
+65 8111 7777 (Orchard) or +65 8111 5777 (Novena)
 Brain & Spine Care
Brain & Spine Care